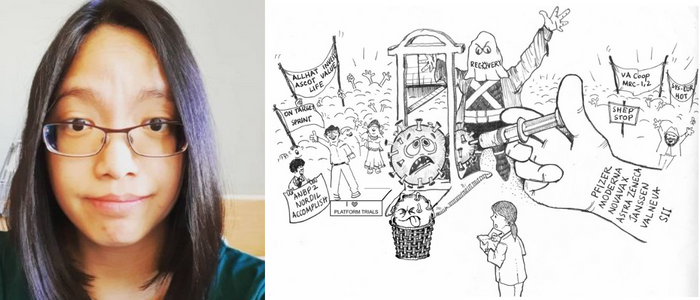
A tale of two diseases article by Dr Stefanie Lip
Published: 16 January 2023
Congratulations to Dr. Stefanie Lip on the publication of her prize-winning essay on COVID-19, hypertension & digital innovation.
A tale of two diseases
Despite its ‘silent killer’ sobriquet, the global efforts to tackle hypertension has been tepid at best. Its insidious impact on humanity over the last century is expected to last far into the future [1]. The initial blaze of research breakthroughs, resulting in the development of antihypertensive drugs supported by the largest clinical trial evidence-base to-date, has faltered. The current state of hypertension research is emblematic of the pondering pace of incremental science, additionally hamstrung by a myriad of diseases competing for finite research funding. In contrast, the response to the COVID-19 pandemic has been the antithesis of hypertension with unprecedented rapid global action bringing the devastating pandemic under control within 2 years—evidently, it was the worst of times and the best of times [2]. In this essay, I shall juxtapose the nearly 2 millennia of hypertension and 2 years of COVID-19 experiences, evoking hidden parallels between the two conditions to glean insights that would effectively direct the use of the £1 million grant to support hypertension research.
It was the worst of times
Since the Yellow Emperor of China noted in 2600 BCE: “[…] if too much salt is used for food, the pulse hardens”, hypertension has grown into a global health crisis affecting over one billion people across the socio-economic spectrum, and directly causing 10.5 million deaths annually (~25000 deaths/day) [1]. Despite the availability of effective and inexpensive antihypertensive drugs only 1 in 5 patients have controlled hypertension and hypertension related cardiovascular death rates have increased over the last decade against previously declining death rates [3]. This highlights an urgent need to rethink strategies to minimise the global burden of hypertension
Early in the pandemic, hypertension emerged as a common comorbidity in patients hospitalized with COVID-19, accompanied by fears that hypertension may increase the risk of severe COVID-19 especially given the key role played by the ACE2 receptor in SARS-CoV-2 virus infection [4]. It became quickly evident that there was no direct interaction between hypertension and COVID-19, but this relief was short-lived. New outpatient visits for hypertension in the US decreased by 39% from 2020 compared with pre‐pandemic figures. The rise of virtual healthcare during the pandemic unintentionally excluded those with lower rates of healthcare literacy or with limited access to internet from chronic disease follow-up. The net detrimental impact on screening/control of cardiovascular risk factors during the pandemic exposed the lack of resilience of healthcare systems for non-communicable diseases, which appears to have caused more deaths than directly from COVID-19 [4]. Over the 2 years from 1st January 2020, there were 6.2 million global deaths directly attributed to COVID-19, but during the same period the excess-mortality is estimated at 13.3–16.6 million(~20,000 deaths/day) [5] – this is strikingly similar to the pre-pandemic daily death toll from hypertension. Those at high cardiovascular disease (CVD) risk (elderly, minorities, socio-economically deprived) are disproportionately affected by COVID-19 [6] and are also dependent on long-term healthcare monitoring, suggesting CVD including hypertension are likely to be the main drivers of the indirect effects of COVID-19.
It was the best of times
Over the last 55 years the pioneering Framingham Heart Study, the Multiple Risk Factor Intervention Trial, the landmark VA Cooperative Study, evidence synthesis by the Prospective Studies Collaboration, and innumerable randomized clinical trials have produced the largest evidence-based underpinning current hypertension management guidelines [7]. Between 1979 and 2007 the age-adjusted mortality rates for stroke and coronary heart disease declined by 57 and 63% respectively, revealing the transformative impact of hypertension research on health.
First published: 16 January 2023

