‘Smart’ 3D-printed braces could improve scoliosis treatment
Published: 7 February 2022
A new type of lightweight 3D-printed back brace capable of sensing how effectively it fits patients could lead to improved treatment for scoliosis.
A new type of lightweight 3D-printed back brace capable of sensing how effectively it fits patients could lead to improved treatment for scoliosis, its developers say.
Scoliosis, a common form of spine deformity, affects around three percent of the population, most often between the ages of 10 and 15. It can be corrected in younger people by a back brace, which is worn until the child stops growing.
While back brace treatment is effective, it can be uncomfortable and can require a time-consuming trial-and-error process to find the best fit for each patient.
A team of engineers and medics from the UK and the United States have combined polypropylene, a lightweight recyclable plastic, with carbon nanotubes to create a cellular material capable of sensing the amount of strain (and stress) it experiences while in use.
The researchers say this material could be used to create a ‘smart’ brace capable of detecting the pressures it applies on the human body, allowing better fine-tuning of the brace and making the process of treatment more comfortable. 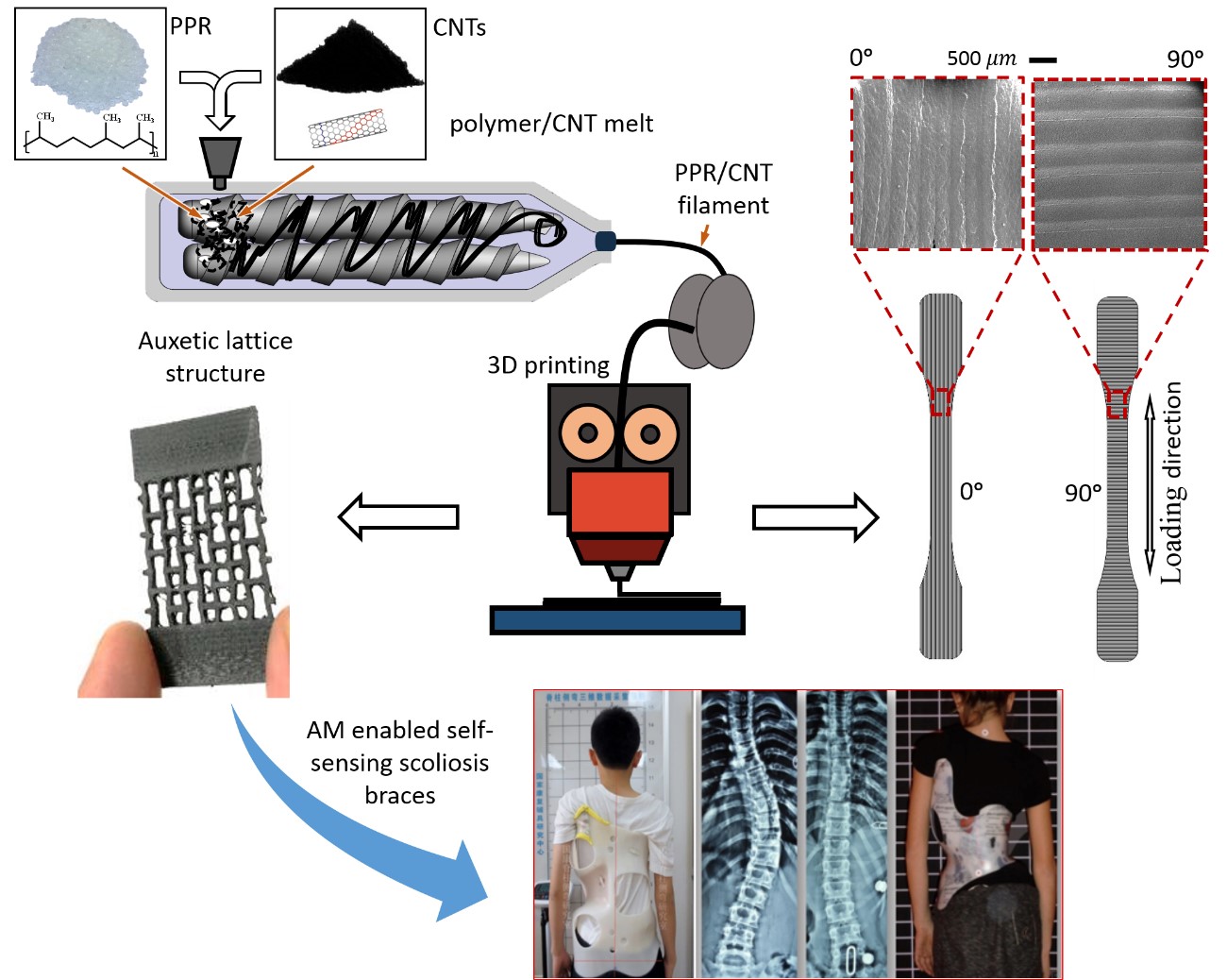
In a new paper published in the journal ACS Applied Materials and Interfaces, the University of Glasgow-led team describe how the carbon nanotubes, placed throughout a material known as polypropylene random copolymer, gave it the ability to form an electrically-conductive network across its structure.
They used 3D printing to create lattice-like structures made from the material and subjected them to static and cyclic loadings, while measuring how the change in electrical resistance of the smart composite under load.
This measure of the material’s changing piezoresistance is what could help to create a smart brace in the future by allowing medics to see which areas of the body are exerting the maximum pressure on the brace.
Their tests showed that, even after 100 cycles of loading and unloading, the material retained its ability to sense the strain experienced by the material, suggesting it could be sufficiently smart to make it suitable for use in a brace.
Dr Shanmugam Kumar, of the University of Glasgow’s James Watt School of Engineering, is the corresponding author of the paper.
Colleagues from Texas A&M University, Massachusetts General Hospital and Massachusetts Institute of Technology in the United States of America also contributed to the research.
Dr Kumar said: “Scoliosis is a painful and debilitating disorder, and while the current generation of braces are better than they have ever been, there is still a lot of room for improvement.
“The self-sensing material that we’ve developed has a great deal of potential to deliver that next generation of improvement. What we hope to see is a future where scoliosis patients can be individually assessed by a doctor and have a 3D-printed brace produced for them which is unique to their condition.
“Then, after a few weeks of wearing it, they can return to their doctor and use the readout from the piezoresistive strain sensing brace to have it adjusted to make it even more effective, without the trial-and-error process that clinicians have to rely on at the moment.
“That could help patients benefit from more accurate adjustments to the stiffness of the bracing in different directions, better data to inform the optimal timing and manner of brace adjustments. That would make them a potentially significant improvement over conventional rigid bracing made from passive materials via conventional manufacturing approaches. Cellular designs of smart composites make the braces lightweight besides offering tuneable mechanical and functional attributes.”
“We’re keen to explore the real-world applications for this technology, and we’re in the early stages of talks with doctors here in the UK and a medical devices company to look at the possibility of trialling these braces in a clinical environment.”
The team’s paper, titled ‘Synthesis and characterization of carbon nanotube doped thermoplastic nanocomposites for the additive manufacturing of self-sensing piezoresistive materials’, is published in ACS Applied Materials and Interfaces. The research was supported by funding from the Abu Dhabi National Oil Company.
First published: 7 February 2022
<< February

